Abstract
Introduction:
Anemia is associated with increased length of stay and mortality in hospitalized patients. Red blood cell (RBC) transfusions could be lifesaving intervention and are generally used as a stabilizing measure until underlying etiology of anemia is identified and corrected. However, RBC transfusions have several adverse effects which occasionally could be life-threatening, including transfusion associated infections, immunologic reactions, volume overload, electrolyte imbalances, and iron overload. The decision on RBC transfusions should be based on patient's clinical status and physician's judgment, supported by data from randomized trials.
Methods:
In efforts to improve RBC transfusion practices in Northern Arizona Healthcare (NAH) facilities, all RBC transfusions between 01/01/2021 and 03/31/2022 were evaluated. Based on randomized clinical trial data, the following RBC transfusion thresholds were considered: Hemoglobin (Hgb) <8 g/dL for hospitalized anemic patients with established cardiovascular disease (CVD) or undergoing surgery, and Hgb <7 g/dL in hemodynamically stable hospitalized patients. Transfusions in pediatric patients, active/suspected blood loss, anemia with hemodynamic instability and massive or recurrent transfusions were excluded from the analysis. For the purpose of this study, RBC transfusion was deemed to be unjustified in cases where only 1 unit of RBC could have been sufficient to raise Hgb level above the specified threshold, however >1 unit was used with no clear justification.
Results:
A total of 2756 units of RBC transfusions were analyzed in hospitalized patients ages 18-102 years. Three patient groups were identified based on the documented provider justification for RBC transfusions: 1) Hgb <7 g/dL, 2) Hgb <8 g/dL with established CVD or undergoing surgery, 3) "other" who did not meet criteria for the previous groups. In the "other" group, the justification was manually entered by the provider.
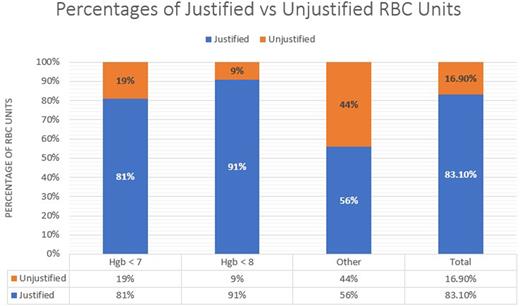
In the Hgb <7 group, 2004 RBC units were transfused in 1019 patients. Of those, 1440 units were transfused for Hgb level of 6.0-6.9 g/dL in 837 patients, with 273 patients receiving 2-4 units of RBCs when 1 unit could have been sufficient to raise the Hgb level >7 g/dL. Therefore, 303 RBC units were considered unjustified. Also, 83 units were deemed unjustified as they were transfused in 72 patients with pre-transfusion Hgb of ≥7.0 g/dL.
In the Hgb <8 group, a total of 711 units were transfused in 500 patients. In the CVD group, 401 units were transfused in 287 patients, of which 260 patients had a Hgb of 7.0-7.9 g/dL. Thirty-four of these patients received 2-3 units when 1 unit was deemed sufficient to increase Hgb >8 (35 unjustified units). Additionally, 5 patients received at least 1 unit of RBC when Hgb was ≥8.0 g/dL (6 unjustified units). In patients undergoing surgery, 213 patients received 310 units. Of those, 150 patients had a Hgb 7.0-7.9 g/dL, 23 of which received >1 units (23 unjustified units).
In the group classified as "other", 41 units were transfused in 39 patients. Hgb levels in this group were between 6.7 to 13.3 g/dL. After further evaluation, 18 units transfused in 17 patients were deemed to be unjustified.
Discussion:
RBC transfusion practices were evaluated in two hospitals in a rural setting in Arizona. From a total of 2756 units, 468 (16.9%) were deemed to be unjustified. The majority of these cases were seen in the Hgb <7 group.
This is the first evaluation of RBC transfusion practices at this institution and a stepping stone to implement measures to improve these practices in the future. The next step includes creating an order set module that would not only require providing justification for blood transfusion, but also confirmation of pre-transfusion and desired target Hgb levels. Additionally, it would implement a notification encouraging single unit transfusions when feasible to decrease transfusion associated adverse reactions and cost burden on patients.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal